Overview
Understanding the potential complications of Coronary Artery Disease is crucial for patients and their loved ones, as it highlights the importance of early diagnosis, effective management, and adopting healthy lifestyle.
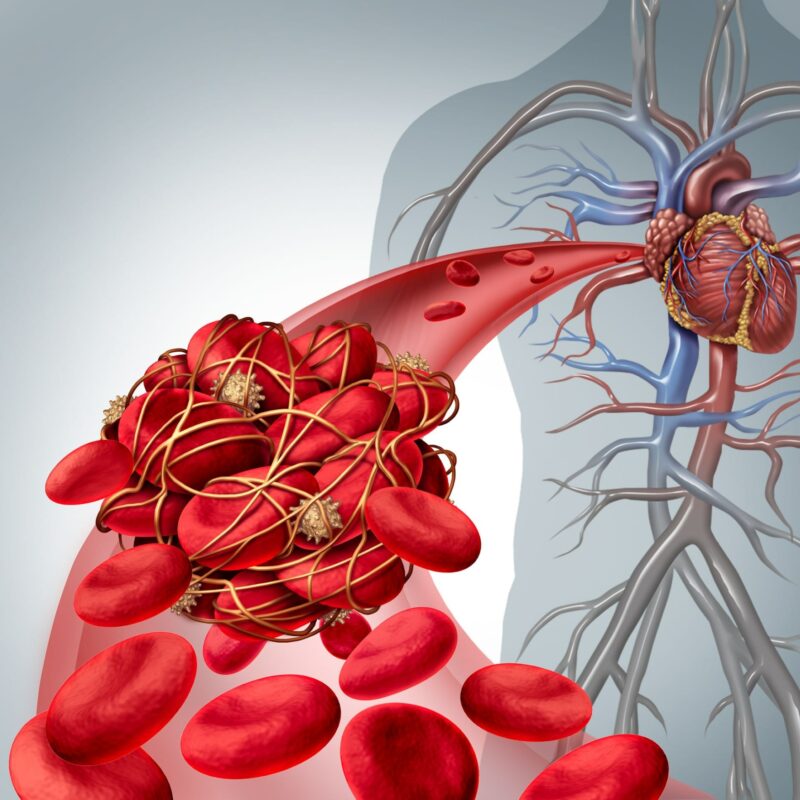
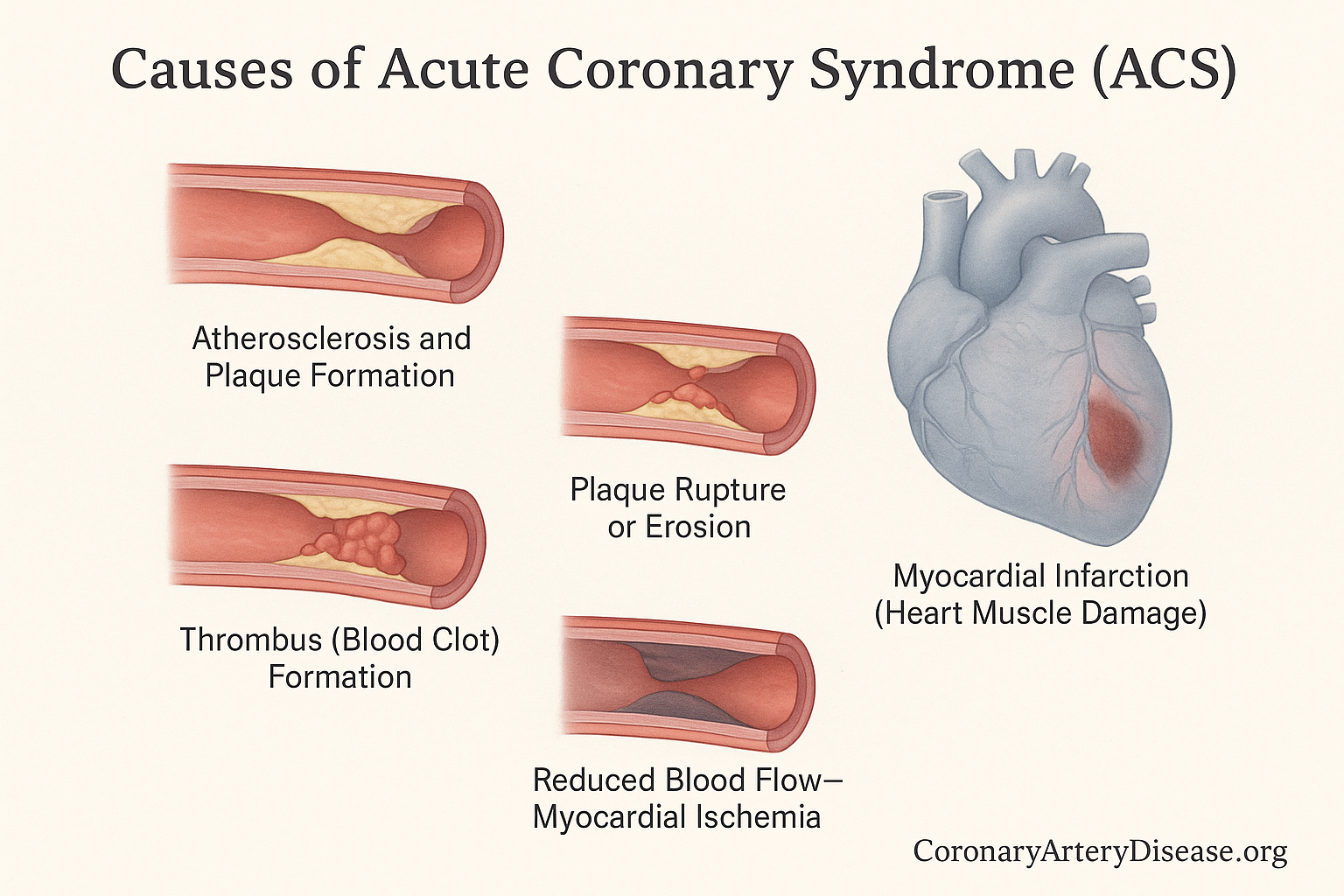
Coronary Artery Disease itself is an atherosclerotic disease, meaning it involves the buildup of plaque inside the arteries, which is inflammatory in nature. This plaque accumulation starts when the lining of the arterial wall is disrupted, leading to lipoprotein droplets gathering in the coronary vessels. Over time, these plaques can disrupt or erode, potentially leading to serious complications.
In Detail
Complications of Coronary Artery Disease
Here’s a quick list of the main complications of Coronary Artery Disease:
- Angina Pectoris (Chest Pain)
- Myocardial Infarction (Heart Attack)
- Sudden Cardiac Death (Cardiac Arrest)
- Arrhythmias (Irregular Heartbeats)
- Heart Failure
- Peripheral Arterial Embolism and Embolic Stroke
The manifestations and complications of Coronary Artery Disease can vary, from less severe symptoms to life threatening events.
Angina Pectoris
Angina Pectoris, or chest pain, is a common clinical syndrome associated with myocardial ischemia. This discomfort can be felt in the chest, jaw, arm, or other areas. While often described as a tight, squeezing, or heavy feeling, its localization can be vague, and there’s considerable individual variation. Angina can be stable, unstable, or even manifest as variant angina (Prinzmetal angina) or microvascular angina. It is important to know that many patients experiencing angina, about half, do not have obstructive coronary artery disease (blockages visible on angiography) but rather have microvascular angina (MVA), which involves problems with the very small blood vessels of the heart, and/or vasospastic angina (VSA), caused by sudden narrowing or spasm of the heart arteries. A critical point is that angina symptoms do not always directly correlate with the severity of the underlying atherosclerosis, and some patients can have considerable myocardial ischemia without any pain, a condition known as ‘silent ischemia’, which is more common in the elderly and individuals with diabetes mellitus.
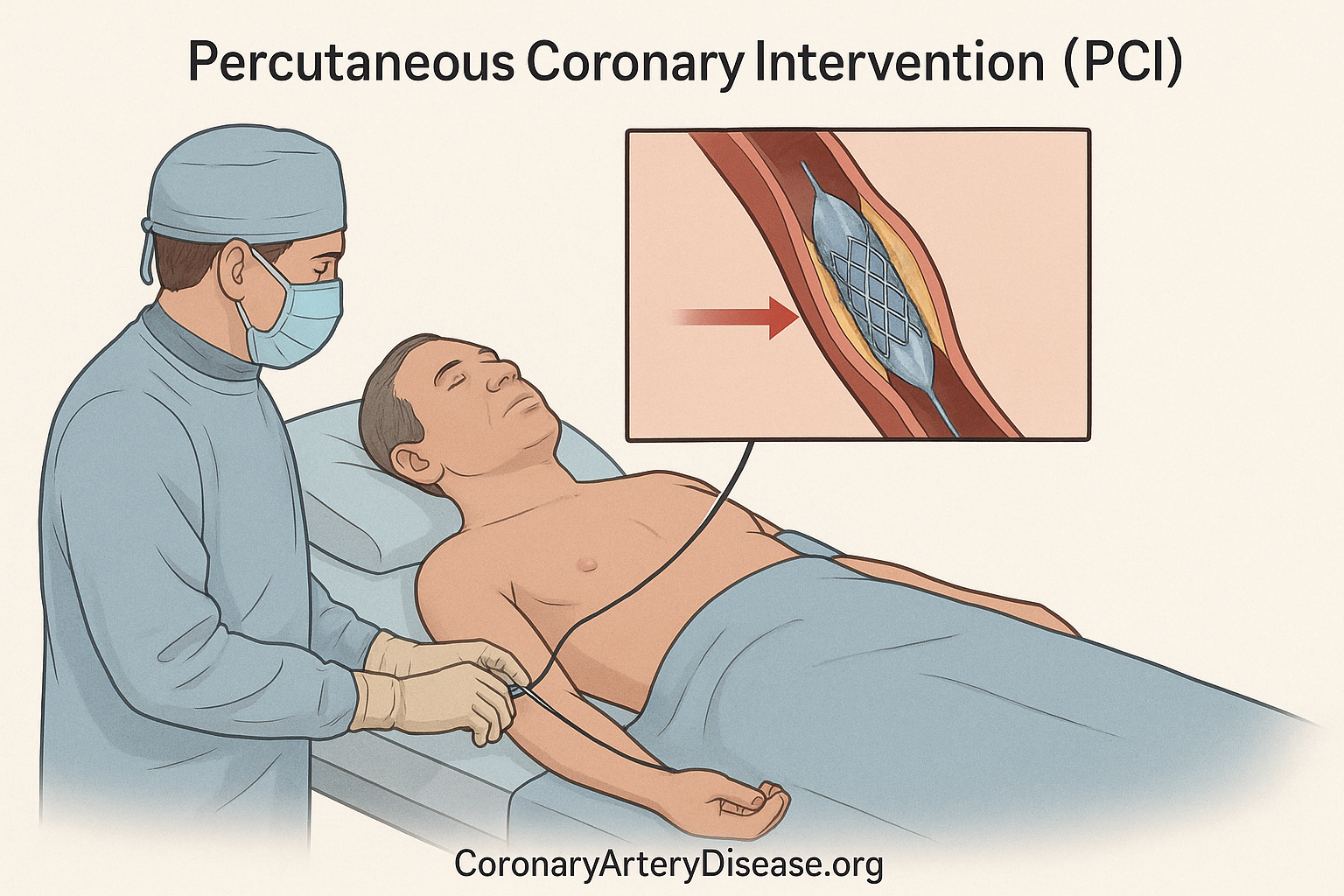
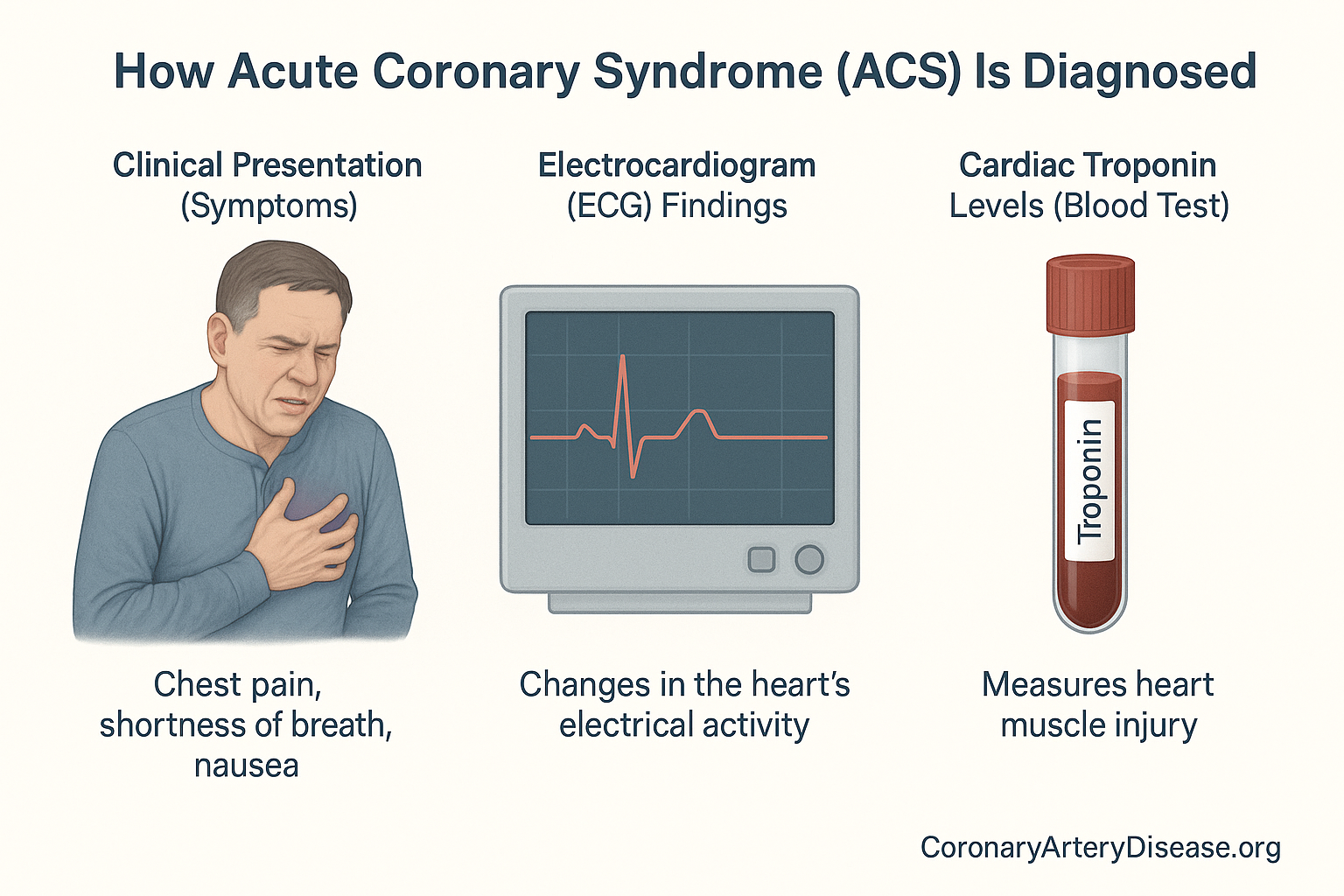
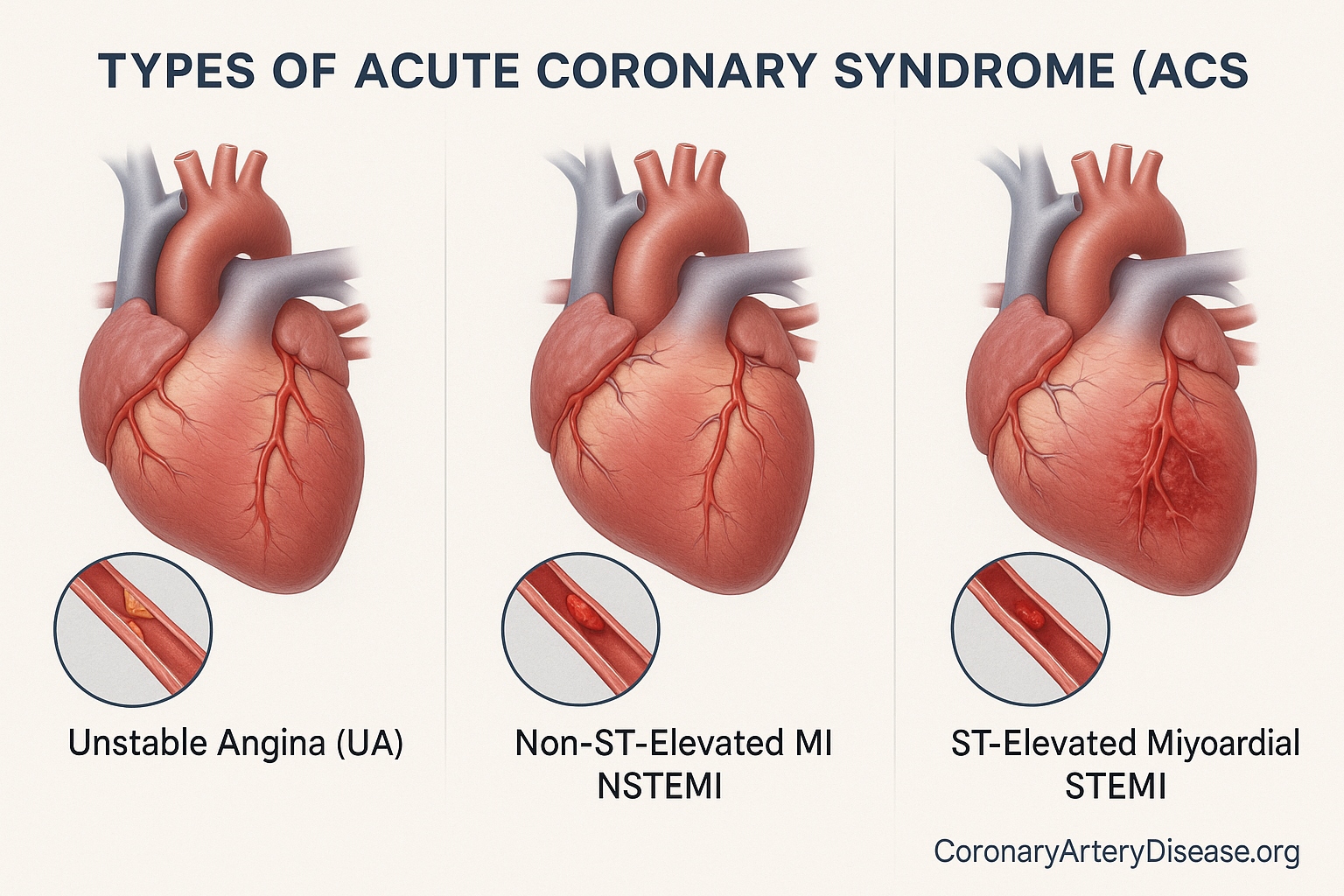
Myocardial Infarction (MI) or heart attack
One of the most serious complications is a Myocardial Infarction (MI), commonly known as a heart attack. This occurs when there is evidence of myocardial necrosis (heart muscle death) due to acute myocardial ischemia, meaning the heart muscle doesn’t get enough blood flow. A heart attack can be classified as either an ST-segment elevation myocardial infarction (STEMI), a severe type where there’s a complete blockage of a heart artery, or a non-ST-segment elevation myocardial infarction (NSTEMI), where blood flow is severely reduced but not completely blocked. For about half of people, a heart attack is the very first symptom they experience from Coronary Artery Disease, and sadly, half of these initial heart attacks can be fatal. Heart attacks are associated with substantial morbidity and mortality and can even lead to mechanical complications such as acute ventricular septal rupture (a hole in the heart wall), acute mitral regurgitation (a leaky heart valve), or free wall rupture. Previous research also indicates that recurrent heart attacks are linked to worse outcomes than the initial event.
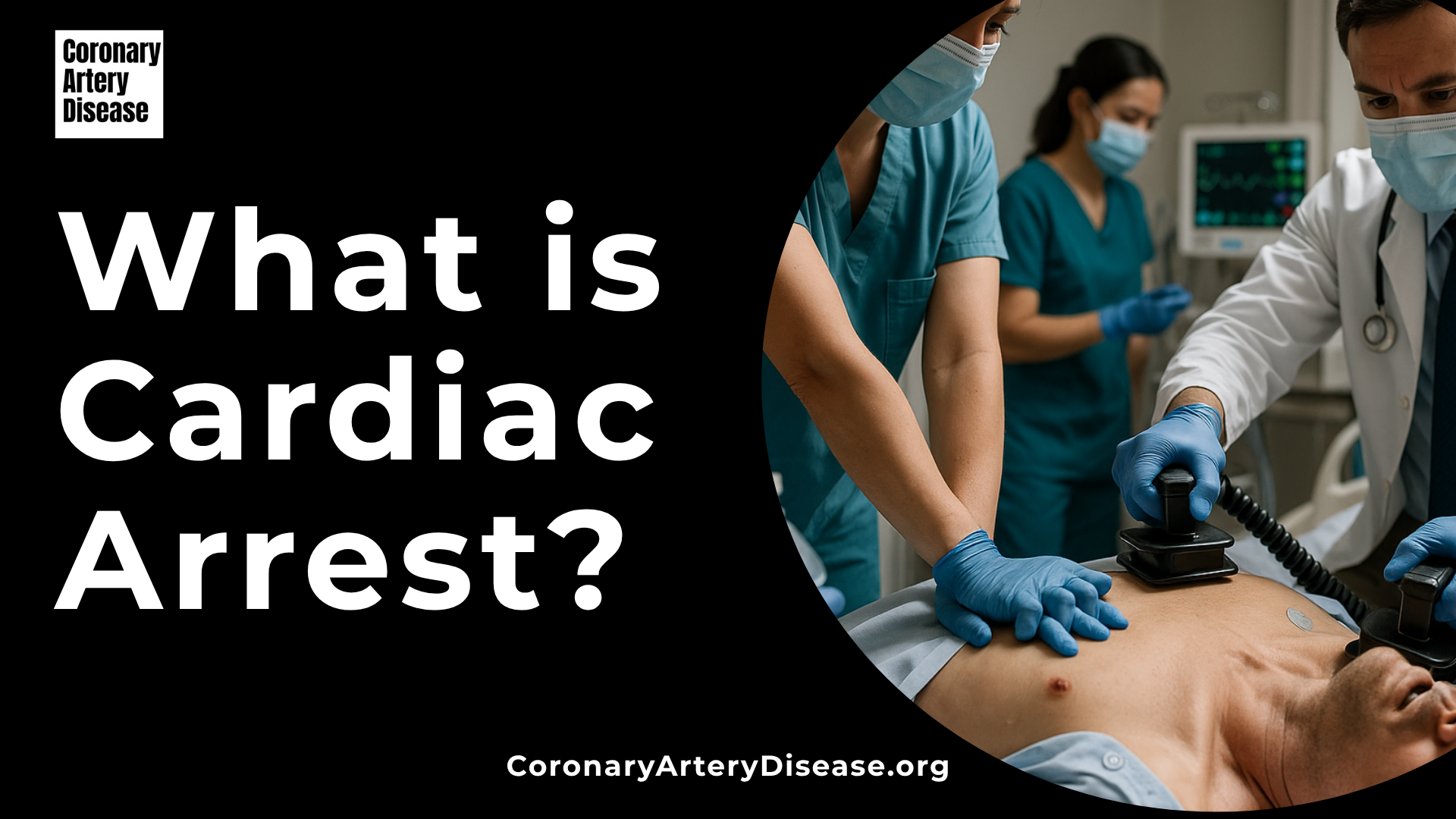
Sudden Cardiac Death (SCD)
Another devastating complication is Sudden Cardiac Death (SCD), also known as Cardiac Arrest (CA). In fact, for one out of four people, sudden cardiac death is the very first symptom of coronary artery disease. Coronary artery disease is the most common cause of cardiac arrest, accounting for over 80% of all cases. The prognosis for sudden cardiac arrest remains poor, with a survival rate to hospital discharge typically between 6% and 10%. Many individuals unfortunately die before even reaching the hospital. Even among those successfully resuscitated, there is a high rate of in-hospital mortality. In survivors of cardiac arrest, a post resuscitation syndrome is commonly observed, which frequently includes transient myocardial dysfunction.
Arrhythmias
Coronary artery disease can also lead to Arrhythmias, which are irregular heartbeats. For instance, atrial fibrillation, a common type of irregular heartbeat where the upper chambers of the heart beat rapidly and irregularly, is observed in 20% of patients with Coronary artery disease. More severe arrhythmias, such as ventricular tachycardia (a fast, abnormal heart rhythm starting in the lower chambers of the heart), can also occur. These irregular heartbeats can sometimes lead to complications like atrioventricular block or, in the most severe cases, sudden collapse and death.
Heart failure (HF)
Heart failure (HF), a condition where the heart cannot pump enough blood to meet the body’s needs, is another common consequence of Coronary artery disease. This often indicates advanced coronary artery disease, perhaps due to a prior heart attack or widespread myocardial fibrosis (scarring of the heart muscle) resulting from previous ischemic episodes.
In some cases, Coronary artery disease may present with peripheral arterial embolism (a blockage of an artery in the arms or legs) and embolic stroke (a type of stroke caused by a blood clot traveling to the brain), typically following a heart attack where a blood clot forms within the heart’s left ventricle.
The pervasive impact of Coronary artery disease extends beyond individual health to society at large. Patients with conditions like microvascular angina and vasospastic angina often experience a profound and long-term impact on their physical and mental well-being, leading to repeated hospitalizations and a reduced quality of life. This underscores the critical need for effective prevention and management strategies.
Other Similar Questions
How does Coronary artery disease affect the body beyond the heart?
Coronary artery disease can lead to issues such as peripheral arterial embolism and embolic stroke, usually after a heart attack. It can also contribute to overall decreased quality of life due to chronic symptoms like fatigue and dyspnea.
Can Coronary artery disease be present without any symptoms?
Yes, it is possible to have significant myocardial ischemia without experiencing any symptoms, a condition known as ‘silent ischemia.’ This is more common in elderly patients and those with diabetes mellitus.
Why is it important for family members to be aware of Coronary artery disease complications?
Because sudden cardiac death can be the first manifestation of Coronary artery disease, and many cases are unexplained even after investigation, family screening for inherited disorders, especially when sudden death occurs before 40-45 years of age, is important to identify at-risk individuals. Awareness of symptoms and risk factors can prompt earlier medical attention.
Resources
- Malakar, A. K., Choudhury, D., Halder, B., Paul, P., Uddin, A., & Chakraborty, S. (2019). A review on coronary artery disease, its risk factors, and therapeutics. Journal of Cellular Physiology, 234(10), 16812–16824.
- Bergmark, B. A., Mathenge, N., Merlini, P. A., Lawrence-Wright, M. B., & Giugliano, R. P. (2021). Acute coronary syndromes. The Lancet, 398(10300), 741–756.
- Smith, J. N., Negrelli, J. M., Manek, M. B., Hawes, E. M., & Viera, A. J. (2015). Diagnosis and Management of Acute Coronary Syndrome: An Evidence-Based Update. Journal of the American Board of Family Medicine, 28(2), 283–293.
- Geller, B. J., & Abella, B. S. (2018). Evolving Strategies in Cardiac Arrest Management. Cardiology Clinics, 36(1), 73–84.
- Granfeldt, A. (2019). In-Hospital Cardiac Arrest. JAMA, 321(16), 1618-1619.
- Krahn, A. D., Tfelt-Hansen, J., Tadros, R., Steinberg, C., Semsarian, C., & Han, H.-C. (2022). Latent Causes of Sudden Cardiac Arrest. JACC: Clinical Electrophysiology, 8(6), 806–821.
- Gallone, G., Baldetti, L., Pagnesi, M., Latib, A., Colombo, A., Libby, P., & Giannini, F. (2018). Medical Therapy for Long-Term Prevention of Atherothrombosis Following an Acute Coronary Syndrome. Journal of the American College of Cardiology, 72(23), 2886–2903.
- Bahit, M. C., Korjian, S., Daaboul, Y., Baron, S., Bhatt, D. L., Kalayci, A., Chi, G., Nara, P., Shaunik, A., & Gibson, C. M. (2023). Patient Adherence to Secondary Prevention Therapies After an Acute Coronary Syndrome: A Scoping Review. Clinical Therapeutics, 45(9), 1119–1126.
- Gaviria-Mendoza, A., Zapata-Carmona, J. A., Restrepo-Bastidas, A. A., Betancur-Pulgarín, C. L., & Machado-Alba, J. E. (2020). Prior Use of Medication for Primary Prevention in Patients with Coronary Syndrome. Journal of Primary Care & Community Health, 11, 2150132720946949.
- Silverio, A., Cancro, F. P., Esposito, L., Bellino, M., D’Elia, D., Verdoia, M., Vassallo, M. G., Ciccarelli, M., Vecchione, C., Galasso, G., & De Luca, G. (2023). Secondary Cardiovascular Prevention after Acute Coronary Syndrome: Emerging Risk Factors and Novel Therapeutic Targets. Journal of Clinical Medicine, 12(6), 2161.
- Fitchett, D. H., Leiter, L. A., Lin, P., Pickering, J., Welsh, R., Stone, J., Gregoire, J., McFarlane, P., Langer, A., Gupta, A., & Goodman, S. G. (2020). Update to Evidence-Based Secondary Prevention Strategies After Acute Coronary Syndrome. CJC Open, 2(4), 402–415.
- Isted, A., Williams, R., & Oakeshott, P. (2018). Secondary prevention following myocardial infarction: A clinical update. British Journal of General Practice, 68(669), 151–152.
- Bavishi, A., Howard, T., Ho-Kim, J., Hiramato, B., Pierce, J. B., Mendapara, P., Alhalel, J., Wu, H.-W., Srdanovich, N., & Stone, N. (2018). Treatment Gap in Primary Prevention Patients Presenting with Acute Coronary Syndrome. The American Journal of Cardiology, 123(2), 237–242.
- Sun, Z. (2013). Cardiac Imaging Modalities in the Diagnosis of Coronary Artery Disease. Journal of Clinical & Experimental Cardiology, S6(e001), 1–4.
- Ford, T. J., & Berry, C. (2020). Angina: Contemporary diagnosis and management. Heart, 106(5), 387–398.
- Libby, P., & Theroux, P. (2005). Pathophysiology of Coronary Artery Disease. Circulation, 111(25), 3481–3488.
- Mayo Clinic. (n.d.). Coronary artery disease – Diagnosis and treatment. Retrieved from.
- Albus, C., Barkhausen, J., Fleck, E., Haasenritter, J., Lindner, O., & Silber, S. (2017). The Diagnosis of Chronic Coronary Heart Disease. Deutsches Ärzteblatt International, 114(42), 712–719.