Understanding The Causes of Acute Coronary Syndrome, is crucial for both patients and their loved ones. It helps explain why the heart acts the way it does during these serious conditions and highlights why quick action and ongoing care are so important.
Overview
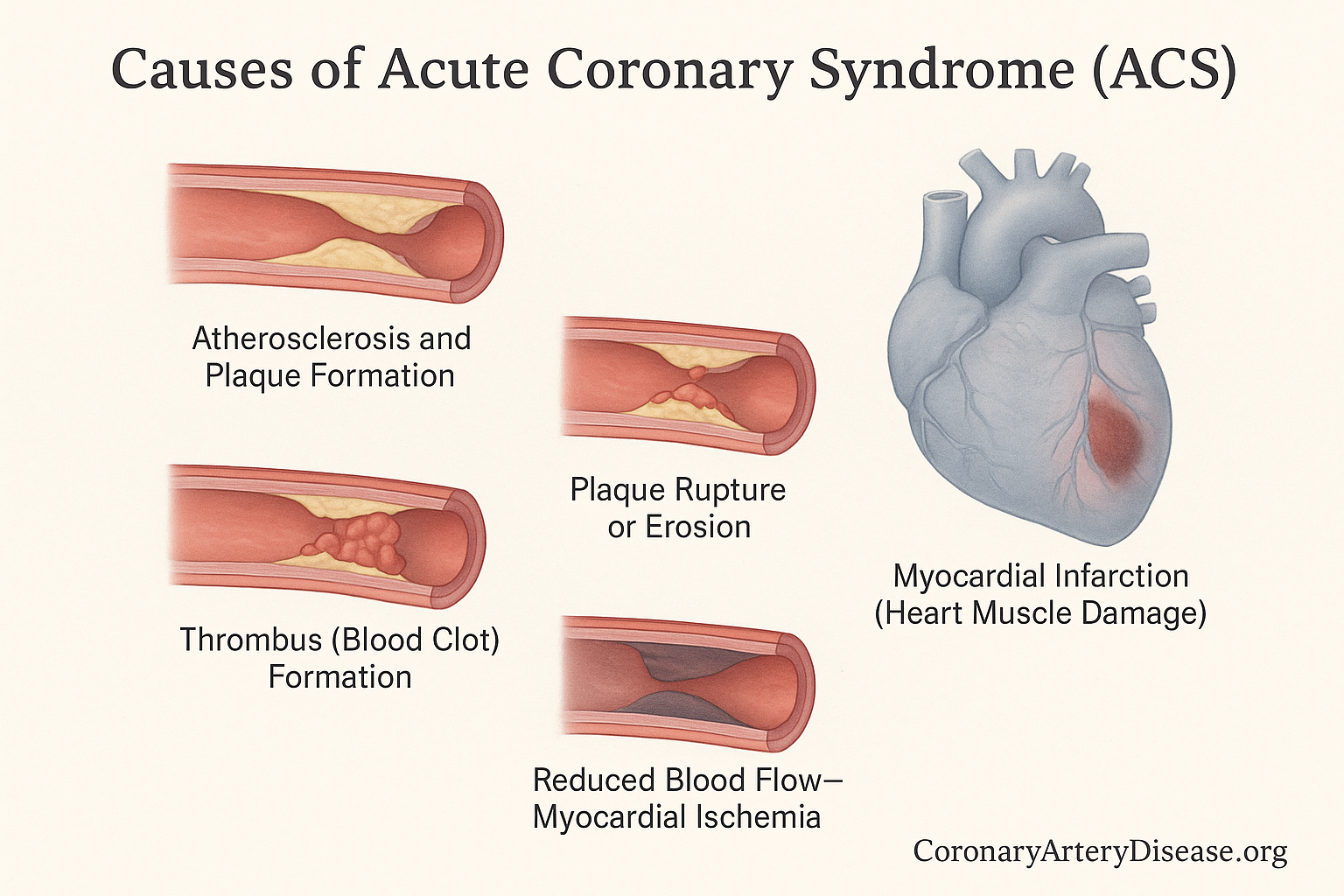
The Causes of Acute Coronary Syndrome (ACS) describes conditions where there’s a sudden, severe reduction in blood flow to the heart muscle. This lack of blood flow means the heart muscle isn’t getting enough oxygen, a condition called myocardial ischemia. If this ischemia is severe or lasts too long, it can lead to myocardial infarction (MI), commonly known as a heart attack, where heart muscle cells are damaged or die. The primary cause of Acute Coronary Syndrome is usually a sudden blockage or severe narrowing in the heart’s arteries.
The core problem often stems from atherosclerosis, a process where fatty deposits build up in the artery walls. When these deposits become unstable, they can trigger the body’s clotting system, forming a blood clot that severely restricts or completely blocks blood flow, leading to the symptoms and damage associated with Acute Coronary Syndrome. It’s important to understand that while this is the most common cause, there are other ways the heart muscle can be injured in Acute Coronary Syndrome.
In Details : The Causes of Acute Coronary Syndrome
First, here’s a quick list of the main mechanisms involved in the pathophysiology of Acute Coronary Syndrome
- Atherosclerosis and Plaque formation
- Plaque rupture or erosion
- Thrombus (blood clot) formation
- Reduced blood flow leading to myocardial ischemia
- Heart muscle damage or death, resulting in myocardial infarction
- Other causes, such as supply-demand mismatch (Type 2myocardial infarction), Spontaneous Coronary Artery Dissection (SCAD), or Myocardial Infarction with No Obstructive Coronary Artery Disease.
The most common way Acute Coronary Syndrome develops is linked to atherosclerosis. This is a long-term process where the heart’s arteries, which are usually smooth and open, become stiff and narrow due to the build-up of fatty deposits, cholesterol, and other substances forming what’s called plaque. When this plaque becomes unstable, it can either rupture (break open) or erode (wear away). When this happens, the body’s natural response is to try and “fix” the injury by forming a thrombus, which is a blood clot, over the damaged area.
This blood clot can suddenly block the artery, significantly reducing or completely stopping the blood flow to a part of the heart muscle. This sudden lack of oxygen and nutrients is what causes myocardial ischemia, leading to symptoms like chest pain. If the blockage isn’t quickly resolved, the heart muscle cells deprived of oxygen begin to die, leading to a myocardial infarction, or heart attack. This process is known as Type 1 myocardial infarction, which is usually what people refer to when they talk about a “heart attack”.
However, not all heart attacks are caused by a sudden clot from plaque rupture or erosion. Sometimes, a heart attack, classified as Type 2 myocardial infarction, occurs due to a severe imbalance between the heart’s oxygen supply and its demand, without a direct sudden plaque-related blockage. This can happen if the heart needs a lot more oxygen (e.g., during extreme stress or a very fast heart rate) or if the body’s oxygen supply is critically low (e.g., from severe anemia or very low blood pressure). Other less common causes of Acute Coronary Syndrome include Spontaneous Coronary Artery Dissection, which is when a tear occurs in the wall of a coronary artery, creating a false channel that squeezes the main blood vessel and reduces blood flow. Another scenario is Myocardial Infarction with No Obstructive Coronary Artery Disease, where a heart attack is diagnosed, but angiography (a special X-ray of the heart’s arteries) doesn’t show significant blockages.
Furthermore, recent insights indicate that infections like COVID-19 can also contribute to Acute Coronary Syndrome by causing direct or indirect inflammation and injury to the heart muscle, or by increasing the risk of blood clots. Understanding these different mechanisms is vital because treatment strategies may vary depending on the underlying cause.
Other Similar Questions
- What is Acute Coronary Syndrome?
- Who is at high risk for Acute Coronary Syndrome?
- What causes a blood clot in Coronary Heart Disease?
- The Diagnosis of Acute Coronary Syndrome?
Resources
- Bergmark BA, Mathenge N, Merlini PA, Lawrence-Wright MB, Giugliano RP. Acute coronary syndromes. Lancet. 2022 Apr 2;399(10332):1347-1358. doi: 10.1016/S0140-6736(21)02391-6. PMID: 35367005; PMCID: PMC8970581.
- Smith JN, Negrelli JM, Manek MB, Hawes EM, Viera AJ. Diagnosis and management of acute coronary syndrome: an evidence-based update. J Am Board Fam Med. 2015 Mar-Apr;28(2):283-93. doi: 10.3122/jabfm.2015.02.140189. PMID: 25748771.