Understanding the treatment and management of Acute Coronary Syndrome (ACS) is vital because it explains the steps taken to address these serious heart conditions and prevent future problems. The goal is to restore blood flow to the heart muscle quickly, minimize damage, and improve long-term health.
Overview
The treatment and management of Acute Coronary Syndrome focus on prompt restoration of blood flow, typically through procedures like coronary revascularization (opening blocked arteries), alongside a combination of medications to prevent blood clots and support heart function. Long-term management, known as secondary prevention, is equally crucial, involving ongoing medication and significant lifestyle changes to reduce the risk of future heart events.
The approach to managing Acute Coronary Syndrome is personalized, taking into account the specific type of Acute Coronary Syndrome, the patient’s individual risk factors, and other health conditions.
In Details
First, here’s a quick list of the main treatment and management strategies for Acute Coronary Syndrome:
- Immediate Assessment and Risk Stratification
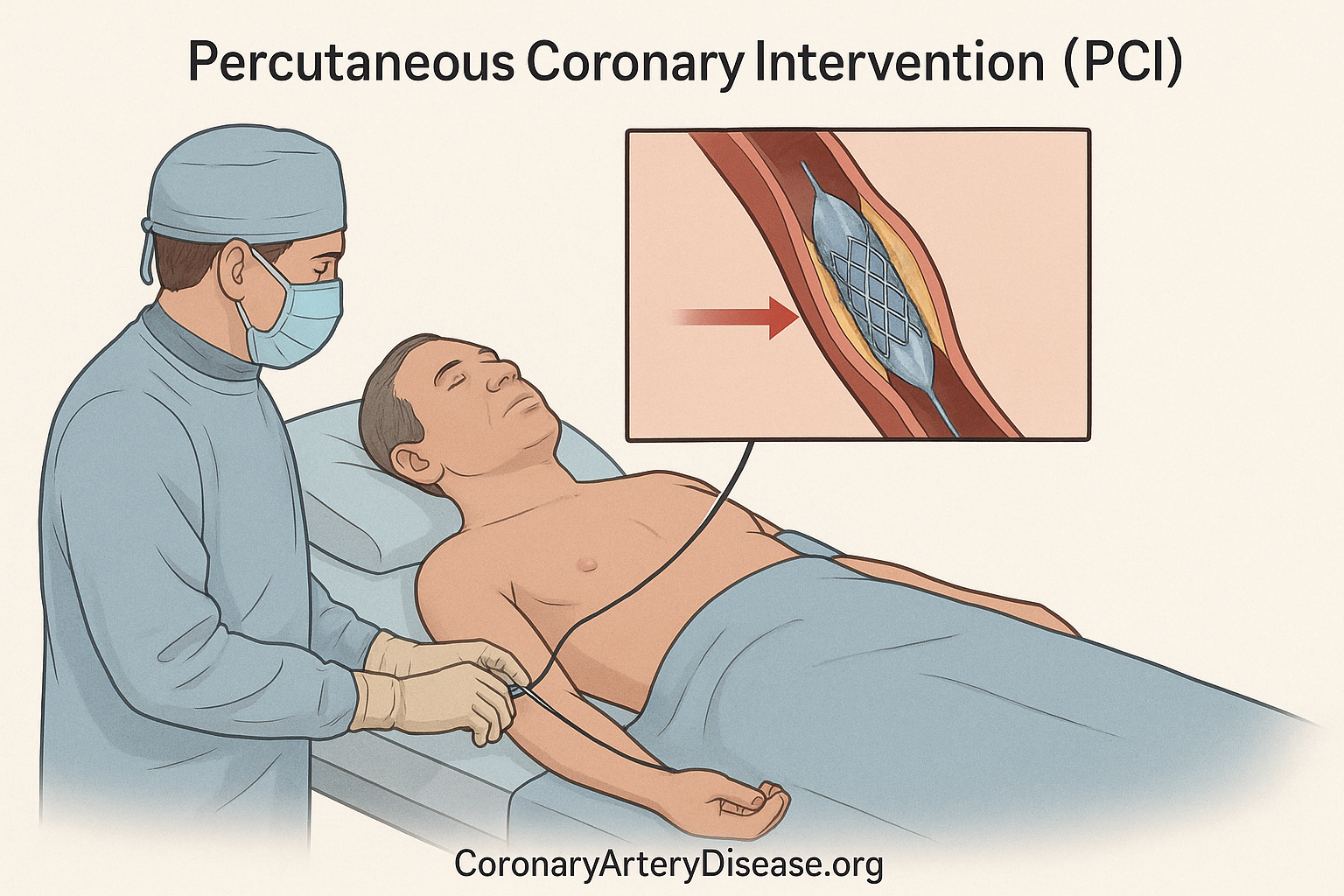
- Coronary Revascularization (e.g., Percutaneous Coronary Intervention (PCI), Fibrinolysis)
- Antiplatelet Therapy (e.g., Aspirin, P2Y12 inhibitors like Clopidogrel, Prasugrel, Ticagrelor)
- Anticoagulation Therapy
- Adjuvant Medications (e.g., Beta-blockers)
- Lipid-Lowering Therapy (e.g., Statins)
- Secondary Prevention (Lifestyle modifications)
- Management in Special Populations (e.g., Women, Elderly, Patients with COVID-19, those in Low- and Middle-Income Countries)
Initial management of Acute Coronary Syndrome
The diagnosis and initial management of Acute Coronary Syndrome begin with a thorough clinical assessment, including a patient’s symptoms, an electrocardiogram (ECG) (a test that records the electrical activity of the heart), and cardiac troponin levels (blood tests that detect proteins released when heart muscle is damaged). These steps help determine the type of ACS and the urgency of treatment. For instance, ST-segment elevation myocardial infarction (STEMI), a severe type of heart attack, is identified by specific ECG changes and requires immediate attention. Prompt evaluation is crucial to prevent potentially fatal outcomes and relieve ongoing lack of oxygen to the heart.
Coronary Revascularization
A key treatment strategy for Acute Coronary Syndrome is coronary revascularization, which aims to reopen blocked or severely narrowed coronary arteries. For patients experiencing a ST-segment elevation myocardial infarction, immediate reperfusion therapy (restoring blood flow) is the top priority, ideally within 12 hours of symptom onset. The preferred method is Percutaneous Coronary Intervention (PCI), often called angioplasty and stenting, which involves inserting a balloon and usually a stent (a small mesh tube) to open the artery. The goal is to perform PCI within 60-90 minutes of the first medical contact. If timely PCI is not available (e.g., if a patient is far from a PCI-capable hospital), fibrinolysis (clot-busting medication) is given within 30 minutes of hospital arrival to dissolve the blood clot. For non-ST-segment elevation acute coronary syndrome patients, the timing of an invasive procedure like angiography (an X-ray of the heart’s arteries) and possible PCI depends on their risk.
Those at very high risk (e.g., unstable blood pressure, ongoing chest pain, life-threatening irregular heartbeats) need emergent angiography within 2 hours. In stable ST-segment elevation myocardial infarction patients with blockages in multiple arteries, opening all significant blockages (complete revascularization) may improve outcomes, but in those with cardiogenic shock (when the heart cannot pump enough blood to meet the body’s needs), only the main blocked artery should be treated immediately.
Antiplatelet therapy
Antiplatelet therapy is a cornerstone of Acute Coronary Syndrome management, working to prevent blood clots by stopping platelets (tiny blood cells that help blood clot) from sticking together. Aspirin should be started as soon as possible after an Acute Coronary Syndrome event and continued indefinitely. In addition to aspirin, a P2Y12 inhibitor is typically added. Common P2Y12 inhibitors include clopidogrel, prasugrel, and ticagrelor. These are usually given for at least 12 months in most patients, as this dual antiplatelet therapy (DAPT) has been shown to reduce future heart problems. While prasugrel and ticagrelor are generally preferred over clopidogrel due to their stronger effects, they also carry a higher risk of bleeding. The choice of agent and duration of dual antiplatelet therapy are carefully considered based on a patient’s individual risk of both clotting and bleeding. Recent studies are also exploring if aspirin can be stopped earlier in some high-bleeding-risk patients after a few months of dual antiplatelet therapy, without increasing the risk of clotting.
Anticoagulation therapy
Anticoagulation therapy, which uses medications to thin the blood and prevent new clots from forming or existing clots from growing, is also critical in the initial management of Acute Coronary Syndrome. Parenteral (injected) anticoagulants, such as unfractionated heparin, low-molecular-weight heparin, fondaparinux, or bivalirudin, are used alongside antiplatelet agents during the acute phase. For patients who also have conditions requiring long-term blood thinners, such as atrial fibrillation (an irregular heart rhythm), the combination of dual antiplatelet therapy and an oral anticoagulant requires careful balance due to an increased risk of bleeding. New oral anticoagulants have been studied in this setting, but while some reduce cardiovascular events, they generally increase bleeding risk and are not yet broadly approved for ACS prevention in Europe or the US.
Adjuvant medications
Beyond these immediate interventions, adjuvant medications play a crucial role in long-term management and secondary prevention. Beta-blockers are usually started within 24 hours of Acute Coronary Syndrome if there are no contraindications, as they help reduce the heart’s workload and oxygen demand. They are typically continued long-term, though the exact duration is debated. Renin-angiotensin system inhibitors (ACE inhibitors or ARBs) are recommended for patients with specific conditions like heart failure or reduced pumping function of the heart (ejection fraction below 40%), as they can reduce mortality. Aldosterone antagonists are also beneficial for certain heart failure patients with reduced ejection fraction and diabetes.
Lipid-lowering therapy
Lipid-lowering therapy is fundamental for preventing future heart events. All patients with Acute Coronary Syndrome should start or continue high-intensity statin therapy to aggressively lower LDL-cholesterol (LDL-C), often called “bad cholesterol”. If the LDL-C target (e.g., less than 1.4 mmol/L) is not reached with statins alone, additional medications like ezetimibe and then PCSK9 inhibitors may be added. These therapies are critical even if initial cholesterol levels seem acceptable, as reducing LDL-C significantly impacts cardiovascular risk. While inflammation is known to contribute to Acute Coronary Syndrome, anti-inflammatory therapies like colchicine have shown mixed results in trials and are not currently broadly recommended by major guidelines.
Secondary prevention
Finally, secondary prevention for Acute Coronary Syndrome patients is crucial and involves both medication and lifestyle modifications. This includes dietary changes, regular exercise, quitting smoking, and participating in cardiac rehabilitation programmes. These measures, combined with adherence to long-term medications, are vital for reducing the risk of recurrent events and improving overall quality of life.
It’s important to recognize that the management of Acute Coronary Syndrome can be complicated by factors such as COVID-19, which can directly injure the heart, increase clot risk, and disrupt healthcare systems. Additionally, sex- and race-based disparities exist, with women and certain racial groups sometimes experiencing delays in diagnosis, less frequent revascularization, and lower rates of receiving guideline-recommended medications. Older patients and those in low- and middle-income countries also face unique challenges and disparities in Acute Coronary Syndrome care.
Other Similar Questions
- Why are statins important after a heart attack? Statins are essential after a heart attack to aggressively lower “bad” cholesterol levels, which helps reduce the risk of future heart attacks and other cardiovascular events.
- What is Acute Coronary Syndrome?
- Who is at high risk for Acute Coronary Syndrome?
- What causes a blood clot in Coronary Heart Disease?
- The Diagnosis of Acute Coronary Syndrome?
Resources
- Bergmark BA, Mathenge N, Merlini PA, Lawrence-Wright MB, Giugliano RP. Acute coronary syndromes. Lancet. 2022 Apr 2;399(10332):1347-1358. doi: 10.1016/S0140-6736(21)02391-6. PMID: 35367005; PMCID: PMC8970581.
- Smith JN, Negrelli JM, Manek MB, Hawes EM, Viera AJ. Diagnosis and management of acute coronary syndrome: an evidence-based update. J Am Board Fam Med. 2015 Mar-Apr;28(2):283-93. doi: 10.3122/jabfm.2015.02.140189. PMID: 25748771.

Leave a Reply