For someone dealing with Coronary Artery Disease (CAD), or for their loved ones, understanding What is the Treatment for Coronary Artery Disease is crucial. The good news is that there are many effective treatments available today to manage the condition and improve how people live with it.
Overview
Treating Coronary Artery Disease involves a combination of procedures to open blocked arteries and various medications that help the heart function better, reduce symptoms, and prevent serious complications like heart attacks. While some treatments can halt the progression of the disease in some cases, the overall goal is to manage symptoms, reduce risks, and improve your long-term health. These treatments range from immediate interventions during a heart attack to daily medications aimed at preventing future issues.
In Details
Here’s a breakdown of the main treatment approaches for Coronary Artery Disease, from direct interventions to daily medications
- Angioplasty and Stent Placement
- Antiplatelet Agents
- Beta-Blockers
- Nitrates
- Calcium Antagonists
- Ranolazine
- Recombinant Fibroblast Growth Factor 2 (FGF2)
Here’s more detail on each of these treatments:
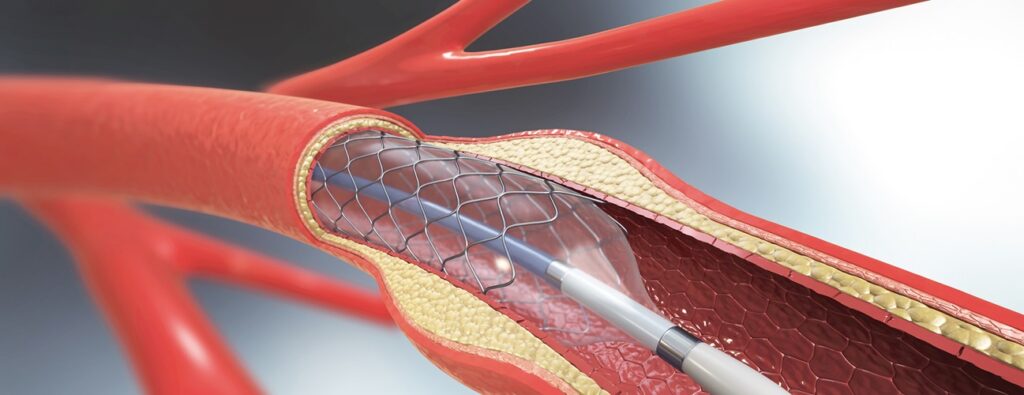
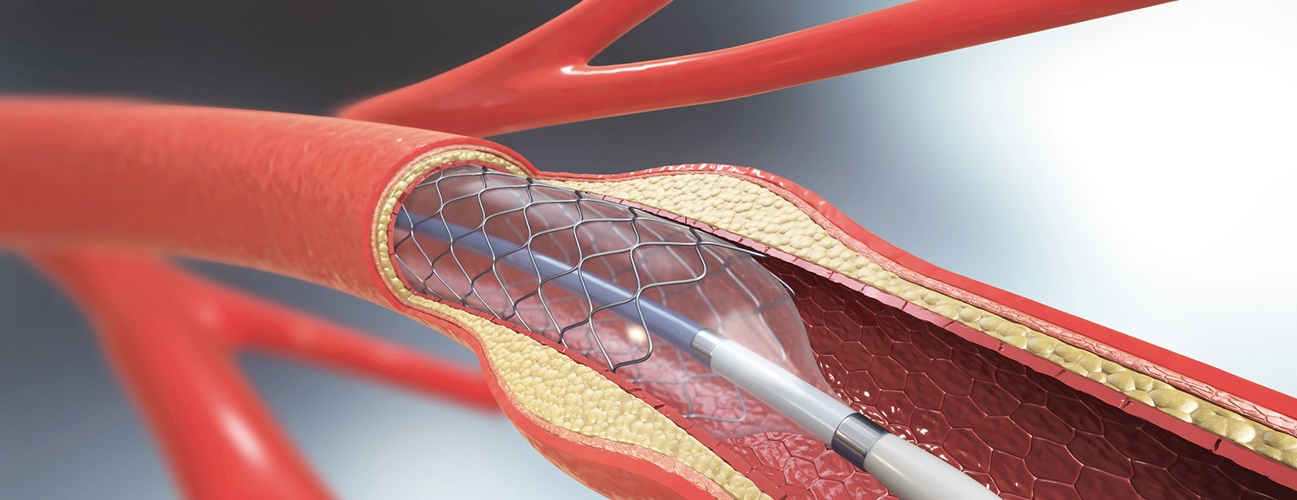
Angioplasty and Stent Placement Coronary angioplasty
Also known as percutaneous coronary intervention, is a procedure often used during a heart attack to quickly open a blocked artery and minimize damage to the heart muscle. This involves temporarily inserting and inflating a tiny balloon inside the clogged artery to widen it. This helps to reduce symptoms like chest pain and shortness of breath. To help keep the artery open and prevent it from narrowing again, a small wire mesh tube called a stent is permanently placed.
Antiplatelet Agents
These are medications, also called antiplatelet drugs, that are crucial in CAD treatment. They work by stopping blood cells called platelets from sticking together and forming harmful blood clots.
Aspirin
Aspirin is a common antiplatelet agent. Regular use by people who have had a heart attack can reduce the chance of future heart-related problems. Aspirin works by inactivating an enzyme (cyclooxygenase-1 or COX-1) that’s needed to form a substance called TXA-2, which helps platelets clump together. By stopping TXA-2 formation, aspirin helps protect against blood clots. Studies have shown that aspirin can significantly reduce the risk of fatal and nonfatal heart attacks or sudden cardiac death in people with stable coronary disease. However, it’s not recommended for people at high risk of bleeding
Thienopyridines
Thienopyridines are another type of antiplatelet drug. These are initially inactive and become active in the liver. They irreversibly block a specific receptor (P2Y12) on the platelet surface, which is important for strong platelet aggregation. Ticlopidine was the first of these, but it was largely replaced by clopidogrel due to side effects.
Glycoprotein IIb/IIIa blockers
Glycoprotein IIb/IIIa blockers are used when platelets are still too active despite other antiplatelet drugs, often because they are less sensitive to them. These blockers are designed to irreversibly bind to and inactivate specific receptors (glycoprotein IIb/IIIa) that are essential for platelets to stick together. Examples include abciximab, tirofiban, and eptifibatide
Other Therapeutic Agents
Beta-Blockers (β-Blockers)
Are given to people with CAD to reduce their heart rate and the heart muscle’s need for oxygen, which helps prevent ischemia (a condition where the heart muscle doesn’t get enough blood flow). These medications can be used to manage angina (chest pain), high blood pressure (hypertension), and heart rhythm problems. They significantly improve angina symptoms by lowering the heart’s oxygen demand and increasing oxygen supply. People receiving beta-blockers have shown better overall prognosis and improved long-term survival, particularly older patients.
Nitrates
such as sublingual nitroglycerin (placed under the tongue) or nitroglycerin sprays, are used for immediate relief of angina. They work by increasing the heart muscle’s oxygen supply and decreasing its oxygen demand. They are often recommended as additional treatment if beta-blockers alone are not enough.
Calcium Antagonists
are medications used to treat coronary vasospasm (a sudden narrowing of the heart’s arteries) and relieve symptoms, often in combination with beta-blocker therapy. They help by both decreasing the heart muscle’s oxygen demand and increasing its oxygen supply.
Recombinant Fibroblast Growth Factor 2 (FGF2)
FGF2 is a type of growth factor that has the ability to stimulate the growth and movement of cells and encourages the branching of blood vessels (vascular tree branching). It works by activating signals through specific receptors, increasing their presence in heart muscle that isn’t getting enough blood, making it more responsive to FGF2 stimulation.
Other Similar Questions
Is Coronary Artery Disease curable?
CAD is typically a chronic condition that can be managed, but its progression can only be halted in some patients through treatments like aspirin, statins, and beta-blockers. Complete “cure” isn’t generally the term used; rather, it’s about effective management and prevention of complications.
Are there side effects to these treatments?
Yes, like all medications and procedures, there can be side effects. For example, aspirin is not recommended for patients at high risk of bleeding. Your doctor will discuss potential side effects with you and weigh them against the benefits.
Resources
For more detailed information, you can refer to the original source:
Malakar, A. K., Choudhury, D., Halder, B., Paul, P., Uddin, A., & Chakraborty, S. (2019). A review on coronary artery disease, its risk factors, and therapeutics. Journal of Cellular Physiology

Leave a Reply