Overview
Atherosclerosis is a chronic, slowly progressing disease where fatty and/or fibrous material builds up in the inner layer of your arteries, called the intima. This build-up forms what are known as atherosclerotic plaques or atheromas, a term derived from a Greek word, reflecting the appearance of the lipid material at the core of these plaques. Over time, these plaques can become more fibrous and accumulate calcium.
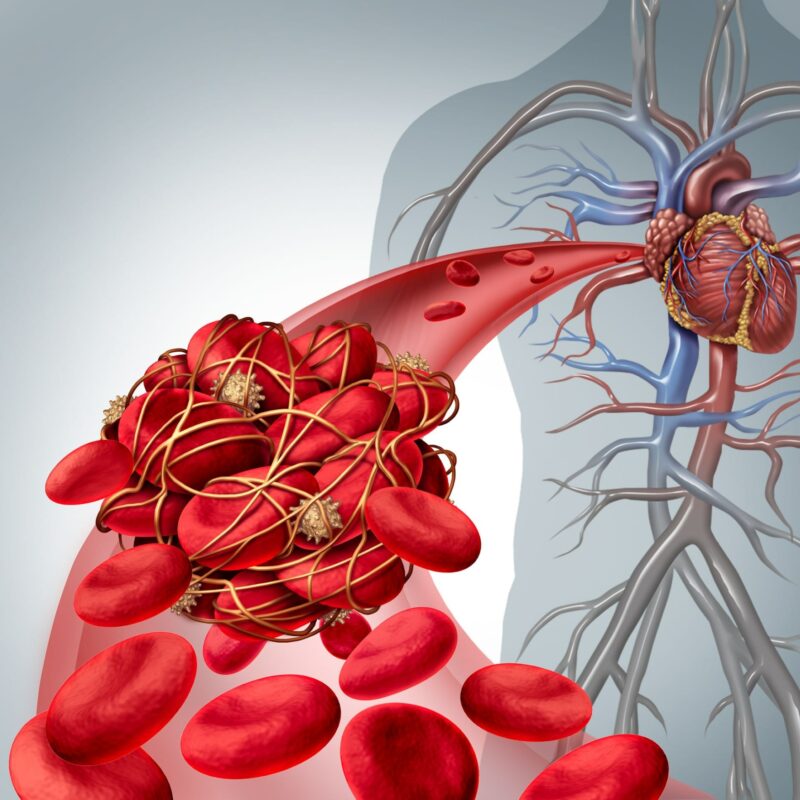
This condition can have serious consequences by impeding blood flow, leading to ischemia (insufficient blood supply to tissues). Plaques can also break open, triggering the formation of a thrombus (blood clot) that can block the artery, causing acute ischemia.
Coronary artery disease (CVD) is a leading cause of vascular disease and death worldwide, significantly contributing to conditions like heart attacks and strokes. Despite advancements in medical care, it remains a major global health challenge.
In Details
First: Key Characteristics of Atherosclerosis
- Build up of fatty and fibrous material: Occurs in the inner lining of arteries.
- Formation of plaques (atheromas): These are the distinctive lesions of the disease.
- Narrowing of arteries: Advanced plaques can reduce the space for blood flow.
- Risk of blood clot formation: Plaques can rupture or erode, leading to clots that block blood flow.
- Involves Low-Density Lipoprotein (LDL): A key factor in plaque development.
- Inflammation and other risk factors: Play significant roles in its development.
Initiation of Atherosclerosis
Atherosclerosis often begins as early as childhood, though symptoms may not appear for decades. The process is thought to start with damage or injury to the inner layer of an artery, called the endothelium. This damage can be caused by various factors, including high blood pressure, high cholesterol, high triglycerides (another type of fat in the blood), smoking or other tobacco use, diabetes, insulin resistance, obesity, and inflammation. When the artery wall is damaged, low-density lipoprotein (LDL) particles – which transport cholesterol through the blood – can accumulate in the intima, the innermost layer of the artery
Research strongly suggests that atherosclerosis would likely not occur if LDL-C (low-density lipoprotein cholesterol) concentrations did not exceed the body’s physiological needs. Prolonged exposure to high LDL-C levels over many years is a primary driver of the disease’s initiation and progression. For instance, individuals with familial hypercholesterolaemia (a genetic condition causing very high LDL-C from an early age) develop premature atherosclerotic CVD, highlighting LDL’s causal role.
Progression of Atherosclerosis
In its early stages, atherosclerotic plaques often expand outwards, away from the arterial lumen (the hollow centre where blood flows), which helps preserve the artery’s width. However, eventually, the growing plaque begins to encroach upon the arterial lumen, leading to stenosis (narrowing) and potentially flow-limiting lesions. This reduced blood flow can cause symptoms like angina pectoris (chest pain from insufficient blood to the heart) during physical exertion.
Complications of Atherosclerosis
The most severe complications of atherosclerosis often arise from the disruption of plaques. The most common trigger for acute coronary syndromes, such as a myocardial infarction (heart attack), is the rupture of an atherosclerotic plaque.
These “vulnerable plaques” typically have a large lipid core covered by a thin fibrous cap (a layer of fibrous tissue). When this cap breaks, the plaque’s thrombogenic (clot-forming) contents are exposed to the blood, rapidly triggering thrombosis (blood clot formation), which can completely block the artery.
Another mechanism, increasingly recognized, is plaque erosion, where lesions without a thin cap or much lipid can also lead to clot formation, particularly in the current era of effective anti-atherosclerotic therapies. These clots can lead to acute ischemic events like heart attacks or strokes.
Other Similar Questions
What are the common symptoms of atherosclerosis?
Mild atherosclerosis often causes no symptoms for many years. Symptoms usually only appear when an artery is significantly narrowed or blocked, or when a blood clot forms. Symptoms vary depending on which arteries are affected. For example, chest pain (angina) if it’s in heart arteries, sudden weakness or trouble speaking if it’s in brain arteries (like a stroke), or leg pain when walking (claudication) if it’s in leg arteries.
Is atherosclerosis curable?
While atherosclerosis is a chronic and progressive disease, its progression can often be prevented, and in some cases, even reversed, through lifestyle changes and medical treatments. Current treatments aim to manage the disease and prevent its serious complications like heart attacks and strokes.
How is atherosclerosis diagnosed?
The diagnosis of atherosclerosis often involves imaging tests that can directly visualise the plaques or assess if there is reduced blood flow to organs. Non-invasive tests include ultrasonography (using sound waves) and CT angiography (a type of X-ray scan).
More invasive procedures like invasive angiography (using a dye to visualize arteries) might be used to guide treatments.
Resources
- “Atherosclerosis” by Peter Libby, Julie E. Buring, Lina Badimon, Göran K. Hansson, John Deanfield, Márcio Sommer Bittencourt, Lale Tokgözoğlu and Eldrin F. Lewis.
- Arteriosclerosis / atherosclerosis