Overview
For many years, doctors and scientists thought that What causes Coronary Artery disease (CAD), often called “heart artery disease,” was mainly too much cholesterol building up in your blood vessels. While cholesterol certainly plays a role, our understanding has changed a lot. We now know that CAD is fundamentally an inflammatory condition, almost like an ongoing battle inside your arteries. This inflammation is crucial at every stage of the disease, from its very beginning to its progression, and even contributes to serious events like heart attacks
.
This new understanding means that managing CAD isn’t just about clearing blockages; it’s also about calming the widespread inflammation that affects your arteries. This inflammatory process can even make non-obstructive plaques, which might not cause symptoms, very dangerous
In Details
The inflammatory process in your arteries starts when the inner lining of these blood vessels, called the endothelium, encounters various “risk factors”. These can include high levels of unhealthy fats like LDL cholesterol, hormones linked to high blood pressure, substances associated with high blood sugar (like in diabetes), or even inflammatory signals from excess body fat. When the artery lining senses these stressors, it becomes “sticky,” expressing molecules that act like hooks. These hooks then grab white blood cells, such as immune cells called monocytes and T lymphocytes, which are circulating in your blood. Once attached, these white blood cells are drawn into the inner layer of the artery wall.
Once inside the artery wall, these immune cells don’t just sit there; they become active participants in a complex inflammatory “conversation” with your artery’s own cells, like endothelial cells and smooth muscle cells. They exchange molecular messages, releasing various inflammatory mediators. These include small fatty molecules (like prostanoids and leukotrienes), other locally acting substances (like histamine), and particularly proteins called cytokines and complement components. These mediators further amplify the inflammatory response, turning it into a persistent state of irritation within the artery.
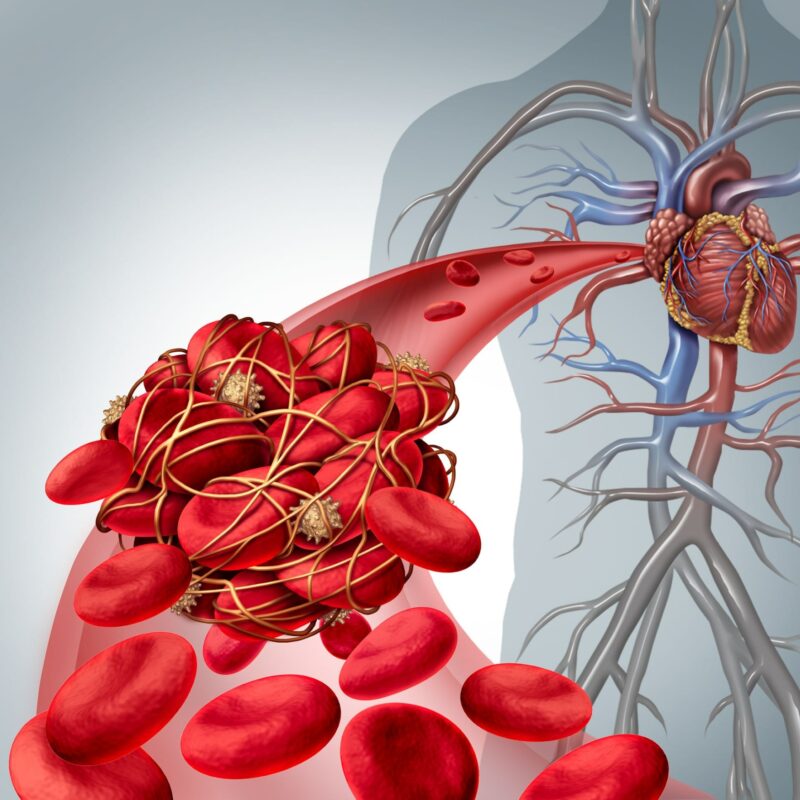
A major consequence of this ongoing inflammation is the migration of smooth muscle cells (SMCs) from a deeper layer of the artery (the tunica media) into the inner lining. These SMCs then multiply and lay down a complex network of structural materials, forming what becomes part of the atherosclerotic plaque. In response to inflammatory signals, these cells also secrete enzymes called matrix metalloproteinases (MMPs), which can remodel or even break down parts of the artery’s structure. Components of this newly formed plaque can bind to lipoproteins, like cholesterol, making them more susceptible to damage, such as oxidation. These damaged lipoprotein products, in turn, continue to fuel and spread the inflammatory response, creating a self-perpetuating cycle of disease. As the plaque grows, dead, lipid-filled immune cells can accumulate, forming a soft, fatty core within the plaque.
This inflammatory process isn’t just confined to one area; recent research shows that it’s often widespread throughout the arteries of individuals who experience acute coronary syndromes (like heart attacks). While some plaques grow inwards and create noticeable blockages, many others grow outwards, a process called “compensatory enlargement”. This outward growth means that a significant amount of disease can be present without causing narrowing that would be visible on standard angiography.
These “hidden” lesions, particularly those with a thin outer fibrous cap and a large lipid core, are very prone to rupture. When such a plaque disrupts, it can trigger blood clot formation, leading to sudden events even if it hadn’t caused any symptoms before. Markers of inflammation, such as myeloperoxidase, have been found to be elevated even in areas of the heart not directly affected by a heart attack, indicating a widespread inflammatory state. This shifts our view from focusing solely on a single “vulnerable plaque” to considering the “vulnerable patient” with diffuse inflammation
Other similar questions
How do specific risk factors, like high blood pressure or diabetes, contribute to inflammation in arteries?
When the inner lining of arteries, the endothelium, encounters risk factors such as high blood pressure (due to vasoconstrictor hormones) or high blood sugar (products of glycoxidation), these cells increase the expression of adhesion molecules
What are the differences between a stable plaque and a “vulnerable” plaque, and how does inflammation play a role?
Stable plaques, often those that cause significant narrowing (stenosis), typically have smaller lipid cores, more fibrous tissue, calcification, and thick fibrous caps2. In contrast, “vulnerable” plaques, which are prone to rupture and cause acute coronary syndromes (ACS), generally have large lipid cores, thin fibrous caps, and are populated by numerous inflammatory cells while lacking relatively in smooth muscle cells (SMCs)
How do medications, such as statins, help by targeting inflammation, not just cholesterol levels?
Statins and similar lipid-lowering therapies contribute to reducing recurrent coronary events by influencing the biology of the plaque, in addition to lowering cholesterol8. These successful therapeutic strategies appear to exert their benefit, at least in part, by combating inflammation8. Specifically, statins can reduce the blood levels of inflammatory markers like C-reactive protein
Resources
The information provided in this summary is based on the following scientific article:
- Libby, P., & Theroux, P. (2005). Pathophysiology of Coronary Artery Disease. Circulation, 111(24), 3481–3488.
This article provides a comprehensive review of the evolution in understanding the mechanisms of coronary artery disease. It is a valuable resource for deeper scientific understanding.

Leave a Reply